Pelvic Organ Prolapse
A prolapse happens because the muscles, tissues and ligaments supporting the pelvic organs (womb, rectum and bladder) become weak.

Childbirth is a common cause of prolapse affecting up to 50% of women. Being overweight, heavy lifting a chronic cough or long term constipation can all cause or worsen a prolapse. It is more common as women age especially after the menopause but rare in women who have not had children.
Symptoms of prolapse
- A sensation of something coming down or out of the vagina
- A visible bulge at the entrance of the vagina
- A sensation of sitting on something ‘like a ball’
- A heavy or dragging feeling in the pelvis
- Leaking urine when coughing, sneezing or exercising
- Difficulty emptying the bowels
- Incomplete emptying of the bladder
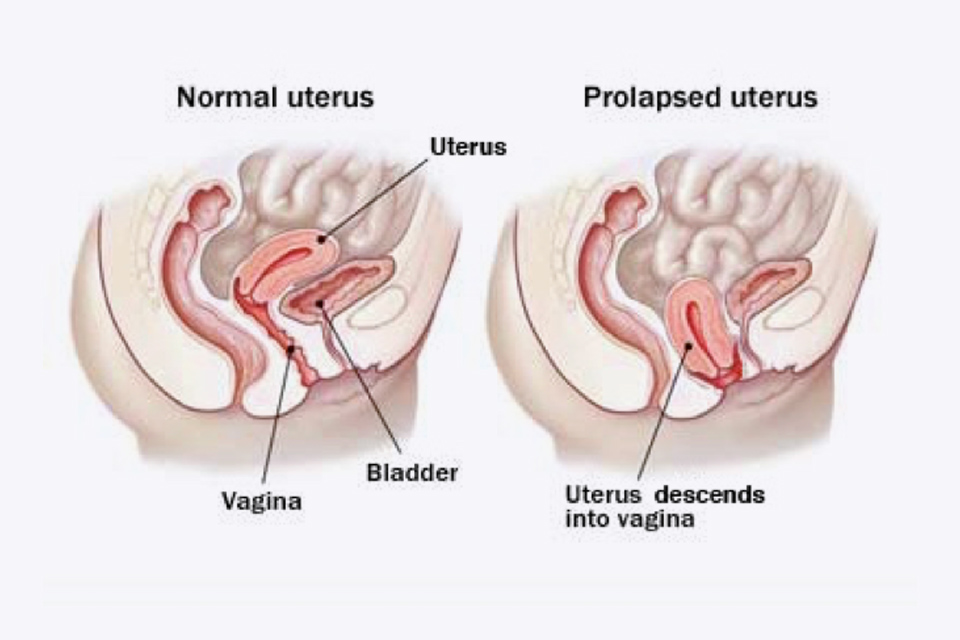
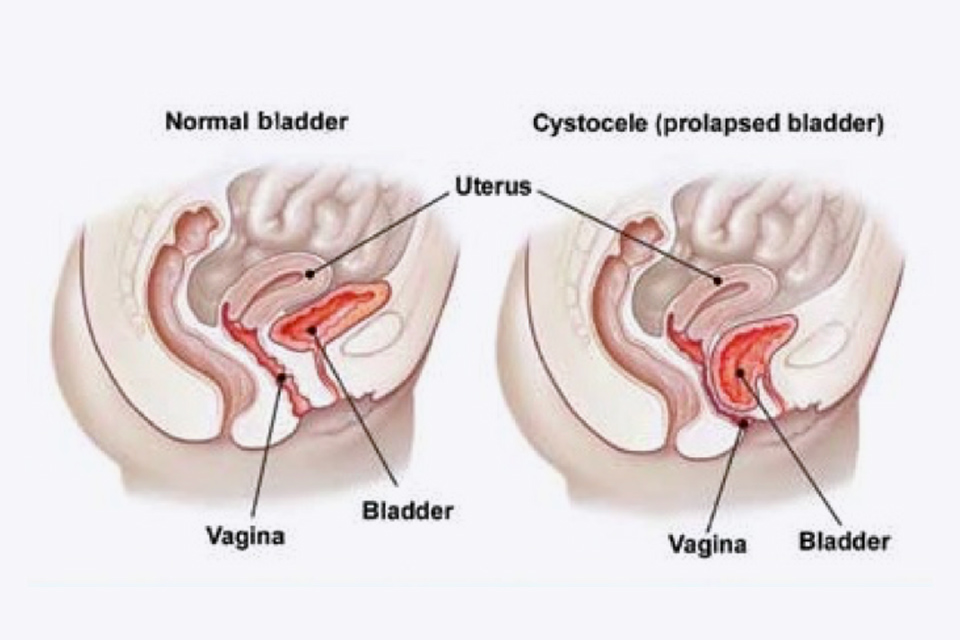
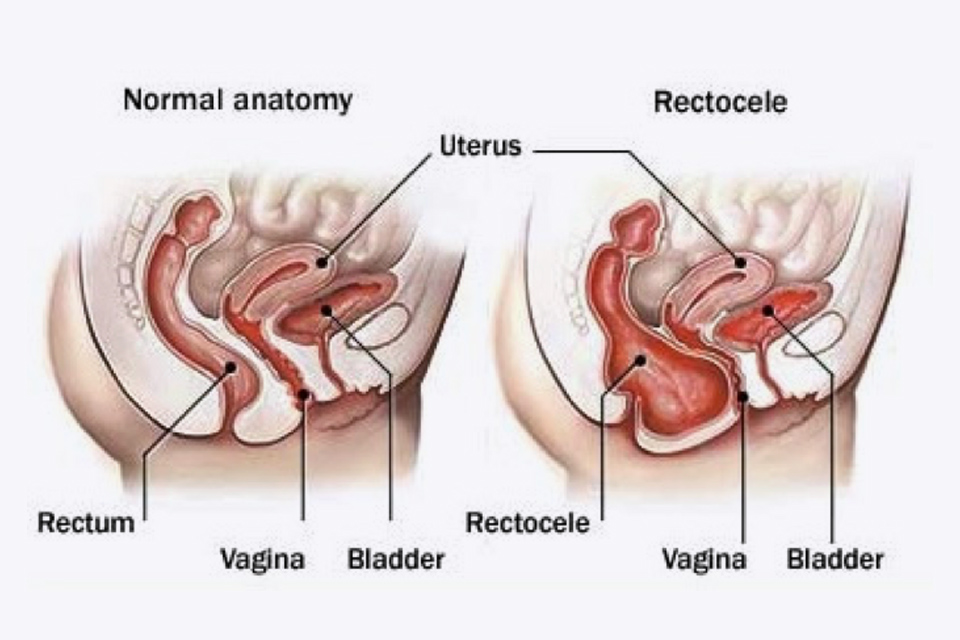
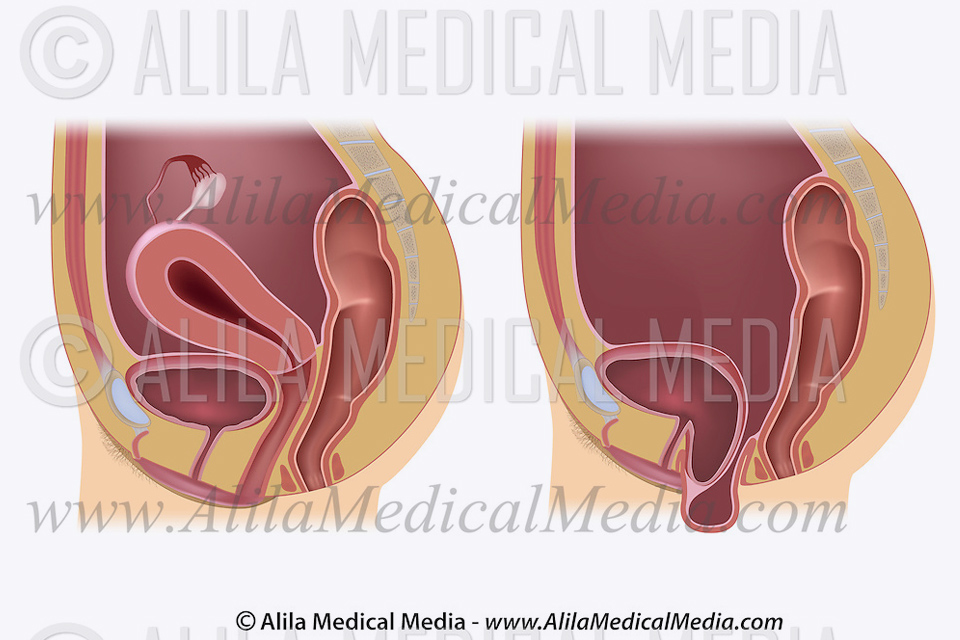
Types of prolapse
A uterine prolapse can be described as mild (1st degree), moderate (2nd degree) where it becomes visible just outside the vagina or severe (3rd degree) where the whole womb comes out of the vagina.
An anterior vaginal wall prolapse (cystocele) causes the bladder to bulge through the front wall of the vagina which can sometimes be seen at the vaginal entrance causing urinary urgency, frequency and incontinence.
A posterior vaginal wall prolapse (rectocele) results in the bowel/rectum bulging forward into the back wall of the vagina causing difficulty emptying the bowel.
A vaginal vault prolapse can be a common problem after hysterectomy. The lack of support where the womb has been removed can result in the top of the vagina sagging down and in some cases bulging out of the vagina.
Treatment of prolapse
Lifestyle changes
Mild prolapse with minimal symptoms probably doesn’t require any treatment. Lifestyle changes such as losing weight, avoiding straining when on the toilet, avoiding heavy lifting and pelvic floor exercises may be all that is required. The use of vaginal oestrogen or even HRT can be very effective in strengthening the pelvic floor and reversing the weakening effect of the menopause.
Pelvic floor exercises
Pelvic floor muscles support the pelvic floor and control the flow of urine from your bladder. They surround the bladder and the tube that you pass urine through (urethra). Having weak or damaged pelvic floor muscles can make a prolapse and urinary leakage more likely. If you only have mild symptoms, doing pelvic floor exercises may help to support your prolapse and resolve urinary stress incontinence. Pelvic floor exercises will generally not help significant prolapse.
If you have mild symptoms of prolapse or urinary leakage I would always recommend a consultation with a specialised pelvic floor physiotherapist who will properly asses your pelvic floor, identify muscle weakness and will then recommend a tailored treatment to maximise success.
Download Pelvic floor exercises
Vaginal pessaries
Conservative treatment can involve inserting a vaginal pessary which is similar to a diaphragm or cap and holds the prolapse in place. They are made of silicone, come in a variety of shapes and sizes and may be suitable if you prefer not to have surgery or are medically unfit to undergo an operation. Once fitted they need to be checked every six to twelve months.
Vaginal pessaries can sometimes cause a discharge, irritation or bleeding, they need to be removed before having sex, which some patients can manage to do themselves. Other potential problems include urinary tract infections, an imbalance in the normal vaginal bacteria (bacterial vaginosis), occasional stress incontinence and difficulty emptying the bowels, generally if fitted correctly many of these problems can be minimised and the pessary is not noticeable.
Surgery
There are a number of different surgical options to repair a significant prolapse and these depend on a number of factors:-
- What type of prolapse is present
- Is there more than one prolapse present
- Has prolapse surgery been undertaken previously
- Are there associated urinary symptoms (stress incontinence, urgency, frequency)
- Is maintaining fertility important (ie avoiding hysterectomy)
Stories
Prolapse of the vaginal wall
Prolapse of the vaginal vault (top of the vagina after hysterectomy)
- Sacrocolpopexy for Vaginal Vault Prolapse
- Sacrospinous fixation (SSF) for prolapse of the uterus (womb) or prolapse of the vaginal vault (top of vagina)

