Urge Incontinence
Urgency is when a patient develops a sudden, compelling feeling that they want to pass urine. Sometimes the urgency can be so powerful that urine starts to leak before reaching the toilet – a condition called urge incontinence.

Common causes of urgency
Often urgency occurs because the bladder is irritable or overactive – a condition known as detrusor overactivity. However, there are a number of other common causes of frequency and urgency:
- Drinking too much (or too little) fluid
- Caffeinated drinks (e.g.) coffee and tea
- On overactive bladder
- Urine infection
- Prolapse
- Lack of oestrogen after the menopause
- Medication (e.g.) diuretics / water tablets
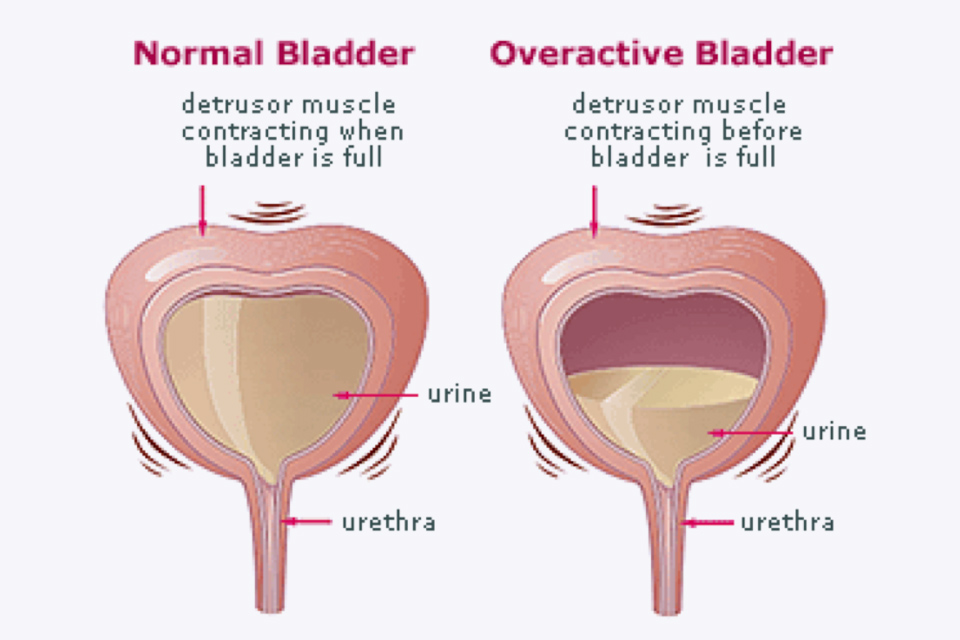
Overactive bladder
No one is sure why an overactive bladder develops. Some patients remember having problems controlling their urine as a child – perhaps they were a late bed wetter, frequently had to leave the class to pass urine while at school or had accidents in the playground while laughing with friends. Other women develop symptoms of urgency as they get older and may find they have to rush to pass urine if they listen to running water, wash their hands or put the key in the door. The urgent and frequent need to pass urine is due to a problem with the muscles of the walls of the bladder (detrusor muscle). The detrusor muscle relaxes to allow the bladder to fill with urine, and then contracts when you go to the toilet to squeeze urine out.
In overactive bladder the detrusor muscle contracts too often, creating an urgent need to go to the toilet, possible causes include:
- Neurological conditions, which affect the brain and spinal cord such as Parkinson's disease or multiple sclerosis
- Conditions affecting the lower urinary tract (urethra and bladder), such as urinary tract infections (UTIs) or tumours in the bladder
- Drinking too much alcohol or caffeine
- Constipation
- Certain medications
Some of these possible causes will lead to short-term urinary urgency and incontinence; others may cause a long-term problem.
Treatment of overactive bladder
Fluid modification. Sometimes patients drink a lot of tea, coffee or caffeinated drinks which may irritate the bladder and make the symptoms of frequency or urgency worse. It is often useful to complete a bladder diary so that we can accurately record how much fluid is taken in during the day, the number of times a patient goes to the toilet and the amount passed each time. Using this information, some women are asked to drink a little more (if they are not drinking enough then the urine can become very concentrated and this may irritate the bladder) or, alternatively, reduce their fluid intake because if they are drinking too much, this may make them go to the toilet even more often.
Bladder retraining. Many patients have got into the habit of going to the toilet "just in case" because they are worried about developing urgency and leaking. Over time this means that the bladder will hold less and less so making the symptoms of an overactive bladder worse. Bladder retraining is used to try and gradually increase the time between visits to the toilet so that eventually the bladder holds more urine and patients gain greater control.
Physiotherapy. Many patients find that pelvic floor exercises, often under the supervision of a physiotherapist, can improve bladder control. As well as strengthening muscles, the physiotherapist will teach some distraction techniques, (e.g.) thinking of work or holiday while you have a strong desire to go to the toilet can make this sensation disappear over 30 seconds or so, and then you can calmly walk to the lavatory.
Medication. Many tablets are available to try and calm the bladder and stop it squeezing when it shouldn't. A patch can also now be used. Approximately 60-70% of patients will gain some improvement with the medication. Unfortunately, it has to be used long term and some patients can develop side effects such as dry mouth or constipation.
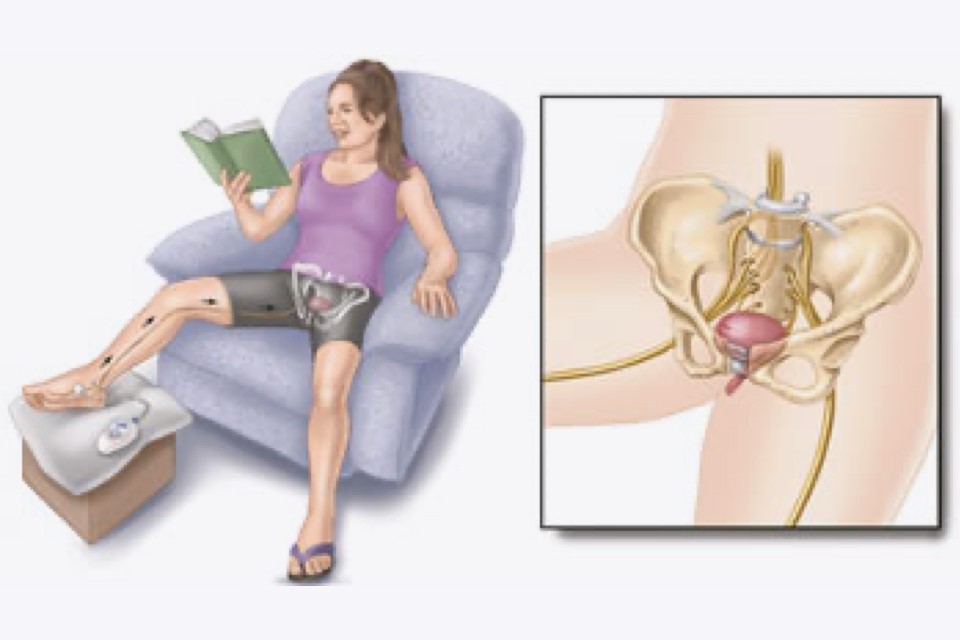
Posterior Tibial Nerve Stimulation (PTNS) is a new treatment for urinary frequency and urgency, most commonly caused by an overactive bladder. It is now available under Mr Broome’s care at the Beaumont Hospital.
PTNS is a form of neuromodulation which can be used with, or as an alternative to, other treatments such as fluid modification, bladder retraining and anticholinergic medication.
The treatment targets the tibial nerve in the ankle and modifies the nerve impulses sent to the bladder which contribute to the development of urgency. A small acupuncture needle is inserted into the ankle near the Tibial nerve and is then connected to a stimulator device.
At the end of twelve 30 minute outpatient sessions, usually undertaken once or perhaps twice per week, there is a 70-80% chance of improvement. Sometimes further "top ups" are given depending upon the initial response. Patients have some slight tingling when the needle is inserted but then do not feel anything while the treatment is taking place.
Side effects are minimal and so far the treatment has been very well tolerated.
Posterior Tibial Nerve Stimulation (PTNS)
Are there people who should not use urgent PC?
- Patients with pacemakers or implantable defibrillators
- Patients prone to excessive bleeding
- Patients who are pregnant or planning to become pregnant during the duration of the treatment
PTNS has recently been approved by NICE and is now one of range of therapies Mr Broome offers for urinary urgency and urinary incontinence at the Beaumont Hospital.
Botulinum toxin A injections
Botulinum toxin A (Botox) can be injected into the sides of your bladder to treat urge incontinence and overactive bladder syndrome (OAB).
Although the symptoms of incontinence may improve after the injections, you may not be able to pass urine normally, so you will be taught how to insert a catheter (a thin, flexible tube) to drain the urine from your bladder. This is called clean intermittent self-catheterisation (CISC) and will need to be carried out by approximately 20% of patients.
Botulinum toxin A is not currently licensed to treat urge incontinence or OAB, so you should be made aware of any risks before deciding to have the treatment. The long-term effects of this treatment are not yet known, but it may be of benefit when other treatments have not worked.
Evidence suggests that botulinum toxin A may cure incontinence or improve symptoms by 90%. The effects can last for up to 12 months.

