What Causes Uterine Fibroids to Grow After Menopause?
Thursday, 15 June 2023
Uterine fibroids are one of the most common issues found in women who are in their most fertile years, age 16-50, and this is because uterine fibroids are dependent on oestrogen. In fact, up to around 80% of pre-menopausal women will get them at some point in their life, and they will experience symptoms ranging from very mild or no symptoms at all to very painful.
During menopause, the ovaries start to reduce the production of oestrogen, and after menopause, production stops altogether as the ovaries, in effect, go into hibernation. This means that a uterine fibroid in a post-menopausal woman is fairly rare. However, there can be instances where these can develop, for example, if you continue to take HRT post-menopause.
It is not exactly clear why uterine fibroids should occur in a post-menopausal woman. What is known is that any symptoms are usually very mild or even non-existent. In most cases of post-menopausal uterine fibroids, your doctor or gynaecologist will likely not recommend treatment unless you are experiencing pain or bladder problems, in which case further investigation would be needed.
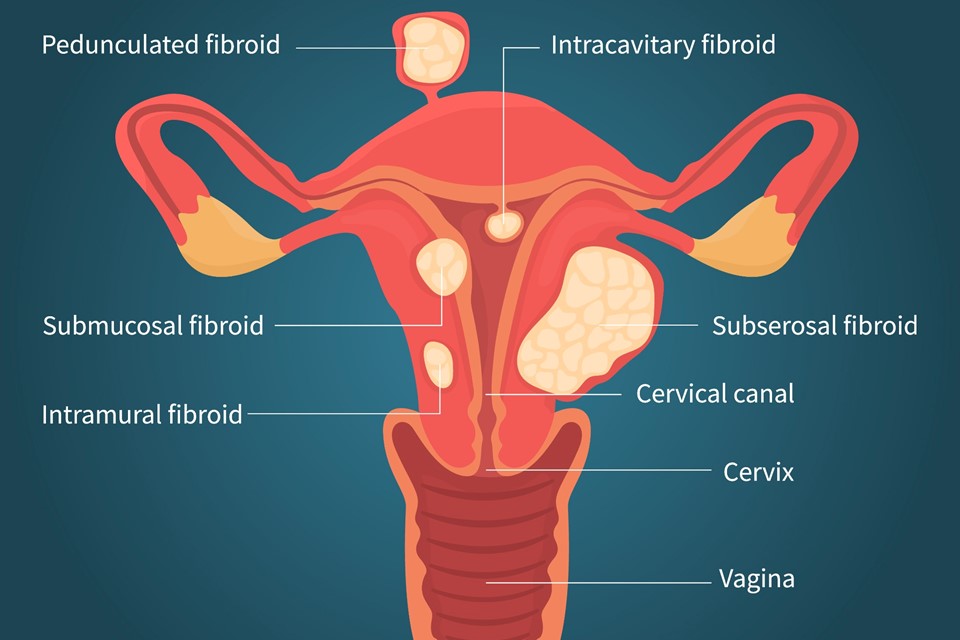
What are uterine fibroids?
They are, it must be stressed, non-cancerous growths made up of muscle and fibrous tissue, which develop in and around the womb and can vary in size.
How are fibroids usually diagnosed?
If uterine fibroids are suspected, your doctor will likely carry out an initial pelvic examination or refer you to the hospital to confirm or rule out fibroids and look for anything else. Occasionally, they may be accidentally discovered during routine tests for other issues.
How do you know if they are fibroids or not?
Some women carry on experiencing heavy bleeding well after other menopause symptoms have been and gone. In most cases, this does not mean that you have developed uterine fibroids or that existing fibroids are getting worse, especially if you have had uterine fibroids in the past. However, it does mean that an investigation is necessary to find out exactly what is going on. These tests may take the form of an ultrasound scan, hysteroscopy, laparoscopy or biopsy and will depend on what your doctor thinks may be the likely cause of your symptoms.
The most common forms of diagnosis are:
Ultrasound scan
This a completely painless scan which uses one of two types to help make a diagnosis; one is a probe which is passed over the skin of your belly, while the other, less commonly utilised, uses a small probe inserted into the vagina. The images are read by a technician on a monitor who can immediately see any signs of fibroids or any other foreign body.
Hysteroscopy
A tiny camera is inserted under local or general anaesthetic through the vagina and cervix into the womb to investigate the interior of the womb.
Laparoscopy
Under general anaesthetic, a tiny camera is inserted through a small incision in your abdomen to allow the internal examination of your womb.
Biopsy
Rarely, a small sample of uterine tissue may be removed, usually during the hysteroscopy procedure, and then sent for examination under a microscope.
Treatment for uterine fibroids
It is rare for uterine fibroids to be present post-menopause and rarer still for any symptoms to be present because any fibroids which were there rapidly shrink after menopause. In almost all of these cases, a doctor will say that no treatment is necessary.
However, if you are experiencing any symptoms such as pain, discomfort or heavy bleeding, these are unlikely to be caused by fibroids, and you should always seek help and advice from your doctor. A specialist like Mr Broome will be able to give you a clear diagnosis and treatment to remedy your symptoms.

