How is a Prolapsed Uterus Treated?
Thursday, 9 March 2023
A prolapsed uterus (womb) is something which affects many women who have given birth, and occasionally women who are in the middle of a pregnancy. It is extremely common post-menopause.
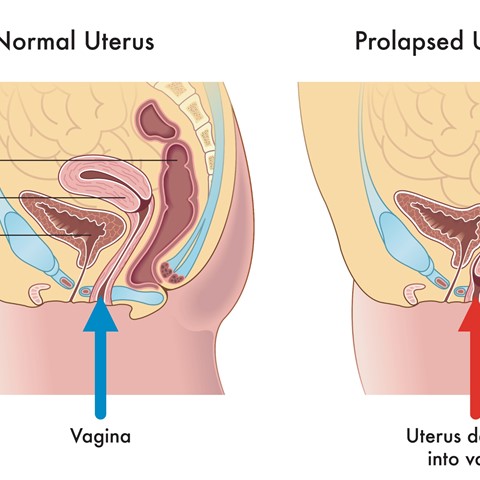
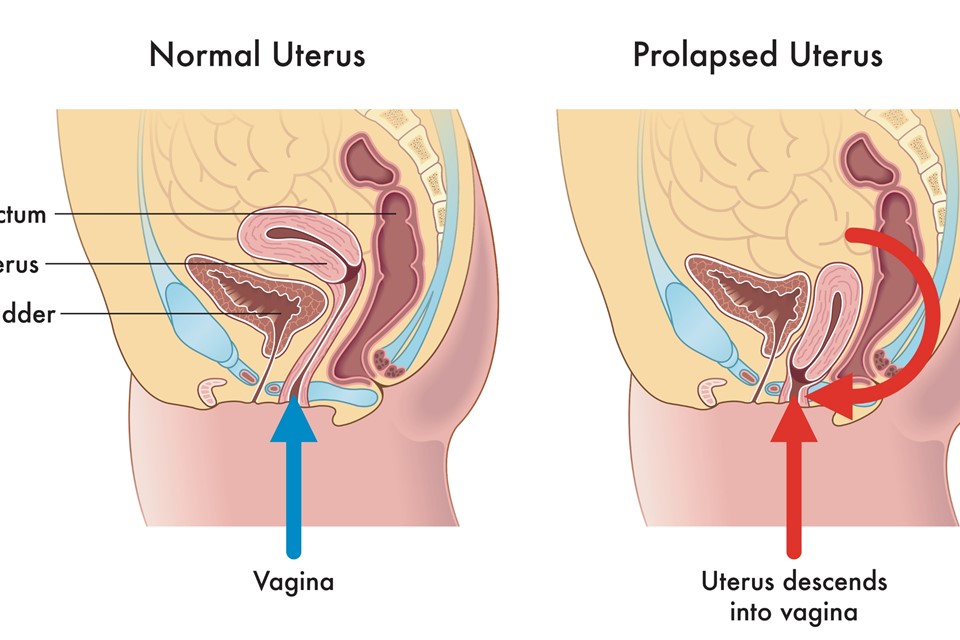
Pregnancy puts a lot of strain on the pelvic floor muscles, tissues and ligaments. This sometimes leads to these structures, which are responsible for supporting the uterus, becoming weak. In some cases, the uterus slips into the vagina and can even protrude from the vagina. A difficult birth can have the same result.
What Does a Prolapsed Womb Feel Like?
You may feel like there is something uncomfortable inside your vagina and you may experience a feeling of heaviness around your lower abdomen. You may feel like you are sitting on a pebble or small ball and you may see a lump or bulge protruding from your vagina.
Fortunately, there are several treatment options available depending on your symptoms and the severity of your prolapse, your age and general health, and whether you’re planning for future children.
Sacrohysteropexy
Depending on the nature of the prolapse and how it is affecting you, your doctor will discuss the suitability of this procedure with you. Sacrohysteropexy can also, in some instances, repair a prolapsed bladder or bowel if either is present with the prolapsed womb.
The operation is performed under a general anaesthetic and is either open or laparoscopic (keyhole) surgery. The difference between these two being the amount of scarring you will have. Open surgery means an incision will be made in the lower abdomen, usually at the bikini line, whilst laparoscopic surgery needs only 3 or 4 tiny incisions.
Laparoscopic surgery is generally preferred and is Mr Broome's chosen method. The advantages are less blood loss, a lower likelihood of wound infection and a shorter hospital stay for the patient. Mr Broome has performed over 300 of this procedures to many grateful ladies.
How is Sacrohysteropexy Done?
A strip of synthetic mesh is inserted to lift and suspend the uterus back in place. One end of the mesh is stitched to the back or around the lower part of the uterus while the other end is attached to the back bone (the sacral promontory). The synthetic mesh will remain inside the body.
An overnight stay is usually required with a temporary urinary catheter in place following the surgery.
You will likely need to take time off work to recover.
Other Treatments for Uterine Prolapse
Not all prolapses need surgery. Mild cases need only advice on lifestyle and health changes. For example you may be advised to:
- Lose weight if necessary and eat high fibre foods to avoid constipation and straining during defecation.
- Avoid lifting heavy objects.
- Stop smoking as coughing can worsen a prolapse.
Pelvic Floor Exercises
These may be recommended to you to try before considering surgery. Pelvic floor exercises can strengthen the pelvic floor muscles and can relieve mild prolapse symptoms. You will receive advice on how to do them.
Vaginal Pessaries
These are available in different shapes and sizes with the most commonly prescribed one being the ring pessary, which allows you to still have sex and get pregnant. A pessary will be fitted by a specialist nurse or gynaecologist.
Hormone Treatment
If you have been through menopause and your prolapse is mild, a course of oestrogen treatment, in the form of a cream, a tablet or a vaginal ring may be recommended.
If you need assistance or advice, Mr Broome at the Spire Manchester Hospital has been helping ladies with prolapse for many years and has seen thousands of successful outcomes. Please e-mail us on info@thepelvicclinic.co.uk or call us on 0161 726 5100.

